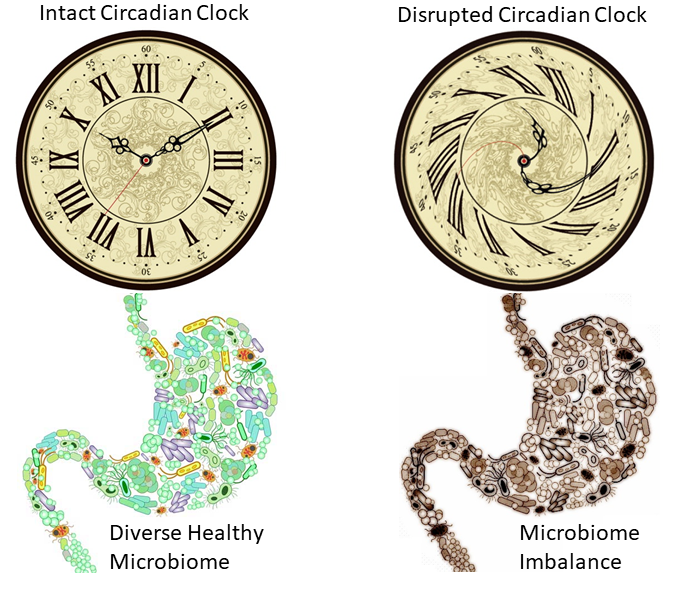
We have known for a while that the population of bacteria in our gut, our gut microbiome, affects the digestive, metabolic, and immune functions in our bodies, but science is showing that it also regulates our sleep and mental states through the microbiome-gut-brain axis. A scientific review study by Rijo-Ferreira and Takahashi published December 2019, discusses how our sleep and wake cycles, also called circadian rhythms, are affected by our genes, by our metabolism, by time-restricted feeding protocols, and by our microbiome.
An earlier review study by Li et al 2018, listed several gut bacteria that affect sleep. For example, some spore-forming bacteria, primarily from the Clostridium genus, modulate the amount of serotonin in the blood. Serotonin is known to promote REM sleep and low levels of serotonin are linked to the development of depression. In addition, Escherichia coli and Enterococcus, which are common in the intestinal tract, also produce small amounts of serotonin. The bacteria Lactobacillus and Bifidobacterium can secrete the neurotransmitter GABA, and abnormal expression of GABA mRNA is often observed in patients with depression and insomnia.
Read more