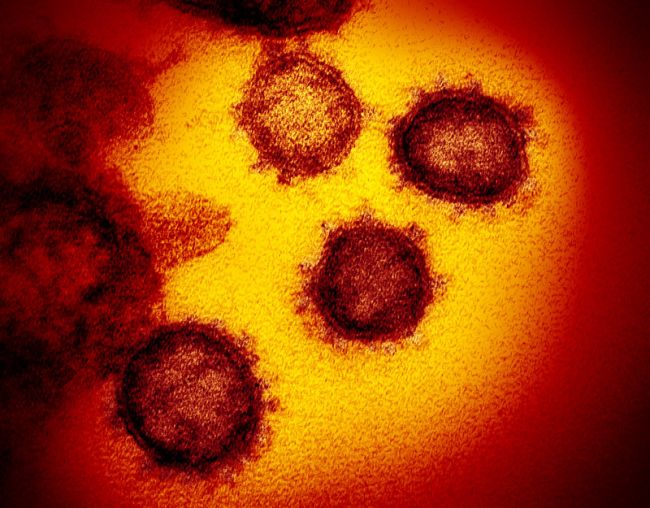
The image shows a transmission electron microscope image showing the new coronavirus emerging from the surface of human cells. (Image: © NIAID-RML)
A study by Shen et al. published on March 9th 2020, has shown by analyzing the lung microbiota (the microbes in the lung) of people infected with the coronavirus SARS-CoV-2, that the virus “evolves in vivo” after infection. “Evolves in vivo” means the virus evolves or mutates inside the body of an infected person during the infection. The virus undergoes a strong immunologic pressure in humans, and may thus accumulate mutations to outmaneuver the immune system. This observation implies that the evolution of the virus may affect its virulence or how it affects a person’s disease progression. This evolution may also affect its infectivity or how quickly the virus can replicate or reproduce itself inside the human body. And it may affect its transmissibility, or how easily the virus can be transmitted to other people.
It is not clear if or how this mutated virus is spread in the population, but the article recommends to strengthen the surveillance of the viral evolution in the population.
In conclusion, this small but significant study of 8 SARS-CoV-2 patients, makes many critical observations related to the quick evolution of the virus, but it suggests that more research is needed to understand what it means for us.
Details About the Study
RNA viruses have a high mutation rate due to the lack of proofreading activity of polymerases, which are enzymes that copy the genome. Consequently, RNA viruses are prone to evolve resistance to drugs and escape from immune surveillance. The mutation rate of SARS-CoV-2 is still unclear, but the study suggests that the mutation rate of SARS-CoV-2 is also comparable to that of the Ebola virus.
The study also found a highly conserved region in the exoribonuclease (ExoN) gene which is a gene that is thought to provide proof-reading activity and that could be a potential target for antiviral therapy.
The authors observed that the SARS-CoV-2 genomes in patients were highly diverse. The high diversity could potentially increase the fitness of the viral population, making it hard to be eliminated. Further studies are needed to explore how this may influence the immune response towards the virus.
The study compared three groups: Patients infected with SARS-CoV-2, patients not infected with SARS-CoV-2 but with community acquired pneumonia (CAP), and healthy people.
Patients with SARS-CoV-2 had the highest proportion of microbial reads compared to CAP and Healthy (SARS-CoV-2: median proportion of 7%, CAP: 0.8%, Healthy:0.1%), which was statistically significant at p<0.001. This means that patients with SARS-CoV-2 have a higher load of microbes than the other 2 groups, and half of those microbes were SARS-CoV-2 viruses. The elevated level of bacteria in the lung microbiome of some COVID-19 patients might increase the risk of secondary infection.
The study found only 2 out of 84 viral sequences in multiple patients, showing that most patients harbor patient specific mutations. They also showed that some nucleotide positions were more prone to mutations and were transmitting in the population, with position 10779 with mutant allele A observed in seven patients.
The number of intra-host variants per individual showed a large variation. They also noted that the number of variations was not relevant to the days after the patient showed the first symptoms nor was it relevant to the age of patients. The authors of the study did not find any reason for the extremely high level of variants in one patient (51 variants). A larger study with more patients is needed to investigate how frequent such outliers are, and whether they are associated with the level of host immune response or the viral replication rate.
The study also looked at the lung microbiota and found that in 6 of 8 SARS-CoV-2 patients, it was pathogen-enriched, and in the other 2, it was commensal-enriched, meaning that it was in a symbiotic relationship with the human host.
Currently, only limited SARS-CoV-2 sequences are shared in public databases but this study shows that there is an urgent need to accumulate more sequences to trace the evolution of the viral genome and associate the changes with clinical symptoms and outcomes.
